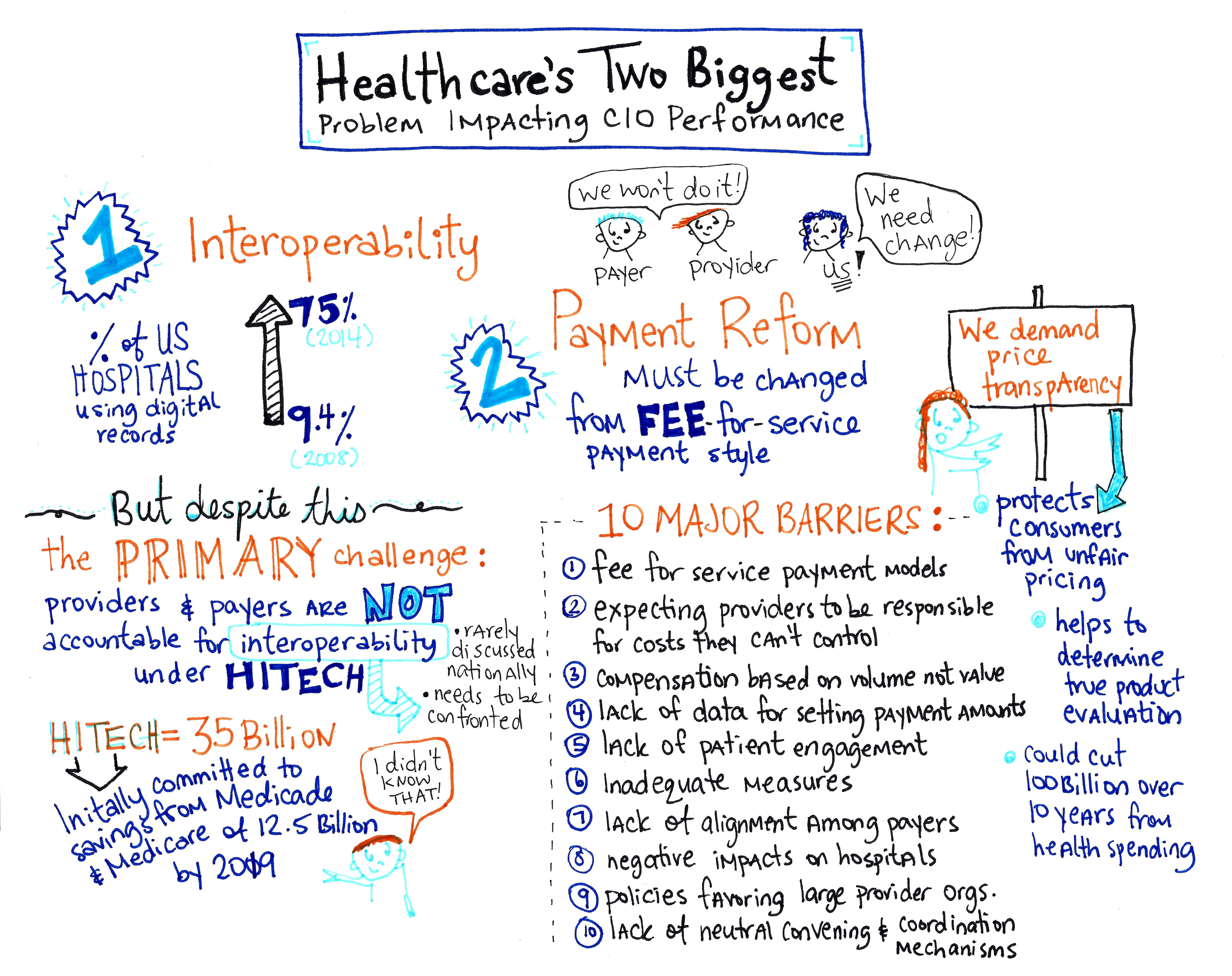
Healthcare’s natural evolution from a fee-for-service to value-based outcome models will remain out of reach, until interoperability and payment reform are removed as barriers to provide patient care.
Interoperability
Overall, it’s widely accepted that the Health Information Technology for Economic and Clinical Health (HITECH) Act, as a policy was a success. It’s not surprising when the percentage of US Hospitals using digital records skyrocketed from 9.4% to 75.5% between 2008 and 2014. However, as we include the patient experience into the definition of success, perspectives change. For example, you have a simple annual checkup at your primary care physician locally, and then a week later you travel to a neighboring town and end up in the hospital. The hospital doesn’t have any record of your recent visit a week ago, no access to labs, and the provider won’t even know to ask unless you mention it. It is an effective meaningful use application? The primary challenge continues to be that providers and payers are not accountable for interoperability under HITEC. The result is a fragmented national healthcare that only hurts the patients we’re trying to help. HITEC was a significant investment with a staggering $35 billion committed for the program. The program initially committed to savings from Medicaid and Medicare of $12.5 billion by 2019. Have the US consumers and patients realized that savings? Why of course not, there is limited interoperability when making clinical decisions with existing EMR technologies. Interoperability is a monumental challenge that is rarely discussed nationally, and needs to be confronted before costs are driven down opening access and allowing providers to explore models for improved quality in patient care.
Payment Reform
The method healthcare providers are paid must be changed from a fee-for-service payment system. Without heavy healthcare payment reform, the realization of better access to higher quality care at lower costs, will not happen. Payers won’t do it. Providers won’t do it. We as patients must spearhead this change. Otherwise, we’ll be passing the burden to the next generation.
The Center for Healthcare Quality and Payment Reform identified ten major barriers of healthcare payment reform 1. Continued use of fee-for-service payment models, 2. Expecting providers to be responsible for costs they cannot control, 3. Physical compensation based on volume not value, 4. Lack of data for setting payment amounts, 5. Lack of patient engagement, 6. Inadequate measures 7. Lack of alignment among payers, 8. Negative impacts on hospitals (inefficiencies), 9. Policies favoring large provider organizations, and 10. Lack of neutral convening and coordination mechanisms. These issues are complex and will require payers, providers and patients all working together for a healthier tomorrow. This realization will be nearly impossible without payment reform considering we have a payment system incented not to keep patients healthy and a dis-coordinated delivery system at the patient level.
In an effort to push down costs, consumers are demanding price transparency. Will healthcare transparency reduce costs? It sounds like it should. Price transparency protects consumers from unfair pricing, and helps to determine the true product evaluation, while building consumer trust. Empowering consumers with price allows, consumers make decisions based on cost and quality information, before care is obtained not after. Better decisions do save money. West Health Policy Institute’s latest analysis indicated, that price transparency could cut $100 billion over 10 years from health spending. However, there can be adverse effects of price transparency, and according to the Health Care Cost Institute, in markets where pricing is very transparent, pricing narrows and the average cost rises. As employers force consumers toward contribution models, selections become difficult and price transparency may not be the single solution. Price transparency creates behavior changes in employees and also in employers. We can only hope the behavior changes in employers soon start to favor the employee.
References
HTA. (2015). Using The PCAT Formula During Conversational Hypnosis To Solve Problems (online image). Retrieved November 15, 2015, from http://hypnosistrainingacademy.com/using-the-pcat-formula-to-help-people-solve-problems-during-conversational-hypnosis/
Peter Nichol, empowers organizations to think different for different results. You can follow Peter on Twitter or on his blog. Peter can be reached at pnichol [dot] spamarrest.com.